Protecting oneself by keeping a healthy body and immune system, as has been determined by research studies, empowers us and gives us hope that we can shield ourselves against the threat of almost any illness that no one ever wants to invite in.
Let’s first discuss how the immune system works and the ways within our control to make sure it’s functioning optimally to help our personal training clients (and ourselves!) stay as healthy as possible.
Understanding Viruses
Let’s talk about viruses since this is what everyone is really most concerned about today. These bizarre pathogens are NOT living cells, they are a packaged set of genes enveloped by proteins. They attack by invading our body’s cells binding to cellular receptors (meant to receive materials intended for our body’s functions), injects its RNA into the cell, and then essentially “pirates” the cell’s organelles to reproduce rapidly. This usually kills that host cell and releases the newly replicated virus bodies into the air when we cough or sneeze.
Jerks.
What makes these offenders particularly difficult to suppress is their ability to mutate more frequently and much faster than most other microbes, like bacteria. This is one of the biggest COVID-19 fears—it’s novel to begin with, and every time it mutates, we have no idea what it will be able to do.
As of right now, most young people have been spared the worst of the symptoms and outcomes, but there are zero guarantees that it can remain so, and in fact, recent days indicate more serious cases are occurring in younger patients.
What we know so far about this particular coronavirus is that it binds to an enzyme of the cell membranes of lung cilia. The cilia are responsible for creating fluid that clears the lungs of unwanted materials. With that function impaired, you get a dry cough—indicating that your lungs aren’t clearing effectively.
How The Immune System Works
We have several lines of defense in the body to defend against “non-self” invaders. The first line is the skin. If something gets past the skin, then the linings of the respiratory system and the digestive passageways may succeed in eliminating them. Beyond that, antigens can be fought in the blood by both clotting processes, and white blood cells and other substances in the blood, which are initiated by the lymphatic system.
The organs of the body primarily responsible for the immune response are the thymus, located at the top of the thorax behind the breast bone, and bone marrow, where early production and selection of lymphocytes take place. Those lymphocytes are then stored throughout the lymphatic system, within lymph nodes, the spleen, the tonsils, and adenoids.
T Cells and B Cells
The stem cells produced in the bone marrow are sent to the thymus to become T lymphocytes or remain within the marrow to become B lymphocytes. There are three types of T cells that perform different functions:
- T helper cells: assist B lymphocytes in antibody production
- T suppressor cells: Kills cells recognized as antigens
- T memory cells: Long-term antigen recognition
On the other hand, B lymphocytes that remain in marrow convert into plasma cells, which produce the antibodies that fight off antigens in the blood.
There are five phases to the immune response:
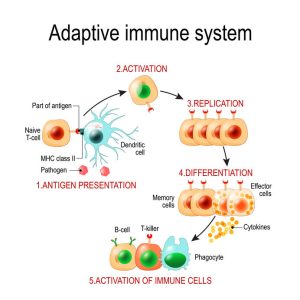
1. Recognition Phase: This occurs when immune receptors on the cell member bind to the antigen, and the antigen is identified as a “non-self” offender. Sometimes the immune system does not recognize an antigen as an offender, which might happen with some viruses, especially novel ones.
2. Amplification Phase: In response to the recognition of an antigen the production of T & B Lymphocytes is ramped up and sent out to battle.
3. Effector Phase: If the lymphocytes are successful, they will kill the antigen.
4. Termination Phase: After the antigen is killed, the immune response is lowered, i.e., production of lymphocytes is decreased.
5. Memory Phase: In order to quickly recognize and kill the same antigen, long-life T memory cells & B lymphocytes are produced.
How The Body Can Be Best Equipped For A Robust Immune Response
Choose The Healthiest Lifestyle Possible
Eat WELL

This may seem a no-brainer but in times of stress, people can make poorer choices in general, but especially with regard to their health choices. Eating a whole-foods diet, rich in colorful, fresh fruits and vegetables, low in processed foods and sugar, and supported by lean proteins (including plant-based proteins) and polyunsaturated fats is the best way to ensure the body is functioning optimally.
Cut the sugar
I hate to think I have to convince anyone why sugar is terrible for your body, but I realize I am being idealistic. Chronic high sugar consumption is associated with obesity, liver damage, gut biome imbalance and increased intestinal permeability (leaky gut syndrome), which causes food material to leak out of the intestines and cause myriad issues. It has also been shown to increase inflammation markers in healthy young men.
We know increased sugar intake spikes insulin, too, which will lead to negative health outcomes including diabetes and obesity. (Btw, the CDC lists a BMI 40 and over as a high-risk factor for COVID-19).
When it comes to illness, if you’re eating sugar you’re feeding the pathogen. Take their food away, and you’ll recovery more quickly.
I personally keep my added sugar intake below 15 grams a day. There are 44 grams of sugar in the average cola. Start reading your labels and you’ll find hidden added sugar in pretty much everything. Keeping your diet close to nature and avoid prepared and boxed foods reduces your intake drastically.
Get moving
If there’s ever a time to emphasize exercise for health it’s now. Moderate exercise has been shown time and again to stimulate the immune system. Studies show respiratory ailments recover more quickly when you stay active, possibly by flushing bacteria out of the lungs and reducing the chances of catching a virus. In addition, increased movement increases body temperature which could help the immune system fight off infection.
If you or your clients don’t have access to the gym or fitness center you’re accustomed to, get creative but get moving. Get outside for fresh air while still being mindful of social distancing.
Get rest
Mysterious circadian rhythms must be optimally maintained for overall functioning, but also influence immune functioning and the development of immunological memory. A lack of sleep increases the likelihood of getting ill after being exposed to a virus, as well as extending illness recovery time.
Adhere to consistent bedtimes and wake times if at all possible. Get ready for bed before you get tired, and stay in bed a bit before jumping out to start your day.
Chill out
And while we’re talking about stress–and this is huge–we all need to manage our stress and anxiety, which can have extremely deleterious effects on the physical health of the body. Not only will stress lower your body’s defenses and make you more susceptible to illness, you will have a much harder time recovering from it as well.
 Please use this time to engage in all the self-care you may have been neglecting. Breathwork, meditation, yoga are all ways to center your mind and calm the body. Take a hot bath with epsom salts, enjoy a glass of wine (not the whole bottle, guys! Let’s all slow down!), healing teas, feel-good movies (maybe avoid watching Outbreak right now), soothing music, nature walks (minding distance to others doing the same).
Please use this time to engage in all the self-care you may have been neglecting. Breathwork, meditation, yoga are all ways to center your mind and calm the body. Take a hot bath with epsom salts, enjoy a glass of wine (not the whole bottle, guys! Let’s all slow down!), healing teas, feel-good movies (maybe avoid watching Outbreak right now), soothing music, nature walks (minding distance to others doing the same).
Sit on your porch if you have one and listen to the spring birds. Love your pets and children. Adopt a pet if you don’t have one (I just got a cat last week!). I also installed a clear birdfeeder that suctions to the window. It took my winged friends more than 2 weeks to notice it, but now we get to watch bird TV, as beautiful bluebirds and golden finches dine right by our kitchen.
Wash your hands!
We all should be washing our hands raw by now. If you leave your home and open your car door, have sanitizer in the car to immediately squirt on. Arrive at your destination and immediately wash your hands if you can, if not, sanitize. Get a grocery delivery or run out for your basic needs? Touch as little as you have to, consider wiping down products with an alcohol wipe before putting them away and avoid touching your face.
These are general guidelines, right? We should all be taking the time to improve our practices and make healthy choices. Want to do more? Here’s what the research says.
Vitamins and Minerals
There exists a synergy of vitamins and nutrients working together to stimulate and support a healthy immune system, including vitamins A, D, C, E, B6, and B12, folate, zinc, iron, copper, and selenium. Most Americans get the recommended dietary allowances of these nutrients, however, evidence suggests that those recommendations are not enough to ensure optimal immune functioning.
Add to that illness, stress, and environmental factors like pollution and toxins in our food, then the need may be even higher. Furthermore, the case may be that several micronutrients are deficient in an individual and immune impairment could occur with even marginal deficiencies.
There is no unanimous agreement on this topic, and contradictions abound, but there is enough evidence in the data to suggest that supplementation with these vitamins and minerals may improve immune function and reduce the risk for disease and infection.
Vitamin C
Vitamin C, or ascorbate acid, is a water-soluble, essential (which means it must be obtained outside of the body since the body cannot manufacture it) vitamin found in high concentrations in citrus fruits and green, leafy vegetables. It is not only crucial for many anabolic functions but it plays a critical role as an antioxidant, which is arguably central to defensive immune system functioning. Further, it helps prevent infections by stimulating the production of antibodies.
Having a C deficiency lowers the immune response and makes one more susceptible to infection. Likewise, taken in copious amounts, this vitamin reduces respiratory and systemic infections. There is much more that gets a bit technical but suffice it to say, vitamin C is a big player in a healthy immune system.
Interestingly, humans are the only mammal who do not manufacture vitamin C in the body. While the USDA has set a daily value set at 70-90mg, there is little detriment to taking higher amounts in the diet or supplementally up to 2 grams, with the exception of mild GI distress. Many proponents of Vitamin C therapy insist there is no danger in exceeding even that amount, and advocate for up to 10 grams of divided doses a day since the body utilizes, depletes, and excretes excess of this vitamin so quickly.
A 2010 study measured serum vitamin C levels in patients following uncomplicated surgeries and found the levels to be very low. The authors speculate the vitamin is used in greater concentrations in order to heal tissue and oxidative damage. Supplementation of 500 mg a day was given to restore levels, while the dosage is recommended to be higher than that for more serious surgeries.
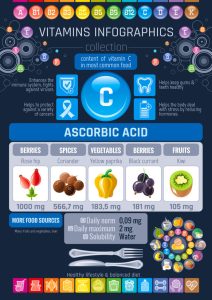
Another study in 2015 supports these findings. The researchers found that critical care patients presented with very low levels of serum vitamin C. Sepsis, trauma, and burn patients were administered high doses of 3 grams a day to restore their serum levels to normal, indicating that when the body is under extreme stress, the recommended daily value is not enough to restore healthy levels.
More relevant to our current situation, a 2020 study published by the Journal of Intensive Care found after reviewing eight trials that large doses of vitamin C (between 1-6 grams a day) shortened mechanical ventilation time by 25%, with the most critically ill patients benefiting the most.
Anecdotally, I have supplemented with C most of my adult life, but have historically waited until illness starts to start dosing. (I take it as
sodium ascorbate which is powdered and can be added to water, purported to be gentler on the stomach and more easily absorbed). I do the same for my children (in addition to a million other things to squash sickness). To this day, none of us has had to go to the doctor for being ill. Yes, we have gotten colds, the flu once a few years ago, and most recently a stomach bug and the weird sinus infection that was going around this winter, but they resolve so quickly there has never been a reason to go in for care.
My children are 3 and 5. I give them up to 500 mg a day and myself 2-3 grams (among many other things). Upping vitamin C intake is the easiest and most effective, yet least risky thing you can supplement for immune function. Hey if it’s good enough for Harry and Megan, it must work, right?
Vitamin D
When you rely on the sun for the main source of a vitamin, expect it to be harder bought in the winter months, when days are shorter and colder, and folks stay inside more. Vitamin D3 is a fat-soluble nutrient manufactured in the skin in response to the UV rays of the sun, but can also be found in certain foods like egg yolks, mushrooms, and fortified milk, but is in highest amounts in cod liver oil and salmon.
Vitamin D works on the immune system mainly through the intestines. It contributes partially by maintaining epithelial integrity and ensuring an appropriate level of antimicrobial peptides in the mucus. Inflammatory Bowel Disease may be associated with impaired Vitamin D signaling in the intestines.
This is a tricky one to take on without medical guidance because over-supplementation of vitamin D is absolutely dangerous. The only way to know if you are deficient in Vitamin D is to get your serum levels tested, and follow your provider’s recommendations to bring levels to normal.
Zinc
This essential micronutrient is required for cell growth, differentiation, and survival. Though it remains unclear as to how zinc functions in the regulation of immune function, the data indicate that deficiency is associated with a dampened immune response.
Adults should get around 10 mg of zinc daily, and it is found in the highest amounts in oysters (not a popular choice, by far), but also in most animal sources. While, zinc is found in whole grain products, nuts, and legumes, those foods also contain Phytates, compounds that bind zinc and inhibit its absorption.
Selenium
This mineral is a potent antioxidant, playing a role in inflammation and the immune response. Many studies have demonstrated the importance of selenium in warding off viruses in particular.
Critically ill patients in Sweden were found to have below threshold levels of selenium, suggesting depletion of the mineral while under physical stress, and were administered the mineral via IV while they remained in ICU. By day 5 in ICU, levels were restored.
Adults need 55 mcg of selenium a day. One Brazil nut contains about twice that! Fish, meat, eggs, cottage cheese, sunflower seeds, mushrooms, brown rice, spinach, and oatmeal also contain a good dose. Eat a well-rounded diet to get all you need. Over-supplementing with selenium can result in toxicity.
Vitamin A
Vitamin A is fat-soluble and has been shown to be a player in the immune system by protecting the epithelium and aiding in mucus tissue production. It has demonstrated anti-inflammatory properties and has assisted in the treatment of various infectious diseases. A deficiency in vitamin A can also disrupt the healthy turnover of bone marrow cells, and thus, homeostasis in the marrow, a primary organ of immune functioning.
Healthy adults require 700-900 mcg of Vitamin A daily. If you want to be set for the week, eat some beef liver, coming in at 6,500 mcg per 3 oz serving. But for most people, one sweet potato will do the trick at 1400 mcg, followed by cooked spinach, carrots, and pumpkin which pack 400- 500 mcg per serving.
Vitamin E
A fat-soluble vitamin, E is another antioxidant show to slow cellular damage. It is important for the differentiation of T cells in the thymus. One review observed that vitamin E plays a role in the immune response, but especially for the elderly.
This is one nutrient where a marginal deficiency can mute the immune response, and the recommended values may be too low. However, it can be found in abundance in most foods of a balanced diet including vegetable oils, cereals, meat, poultry, eggs, fruits, vegetables, and wheat germ oil.
Vitamin E and C co-administered intravenously significantly improved outcomes of patients with lung contusions by tempering the inflammatory response, illustrating the power of synergy when taking all factors into account.
Nutritional Superfoods That Strengthen The Immune System
While there is currently no conclusive evidence that ANYTHING can prevent or cure COVID-19 there is little harm in taking in the foods, vitamins, minerals, and compounds that are proven to be safe, while also demonstrating powerful effects to bolster the body’s immune response.
Garlic
Growing up in an Italian-American household, there wasn’t much that didn’t include garlic. This root’s rich, pungent flavor not only lends depth to cuisine, but it seems to yell, “I’m healthy!! I can kill bad things!” Garlic has been studied to demonstrate strong anti-viral and anti-bacterial action. The compound allicin found in garlic has been shown in lab and human studies to ward off viral activity. Cooking garlic seems to reduce the potency of this effect. Slicing increases allicin activity. If you must cook it, let it sit for ten minutes before heating.
I have literally cut up cloves of raw garlic and swallowed them like pills when ill. This method is not for the faint of heart but stands the best chance for high potency.
Raw Honey
You may have heard consuming local, raw honey is great for seasonal allergies. I’ve also used it to heal minor burns. Honey is close to being magical thanks to the bee pollen that is in it. Both pollen and propolis (the gooey substance bees make from tree sap to construct their hives) have extraordinary properties that are conferred to raw honey.
Here are some of the other benefits that have been reported:
- Antifungal
- Antimicrobial
- Antiviral
- Anti-inflammatory
- Anticancer immunostimulating
- Local analgesic
There are even more stunning benefits, such as treating respiratory infections and coughs, and demonstrating the same anti-inflammatory response as NSAIDS, that I encourage you to read more about if you have the time.
Cocoa Extract
Yes, the same basis of your favorite chocolate treats can be helpful in activating your natural immunity. Cocoa extract was prepared in this study by treating defatting cocoa powder with boiling water (like hot chocolate). The preparation was found to inhibit influenza infection in canine kidney cells. No, not a human study, but it’s reasonable to infer it would have the same effect in any mammal susceptible to the flu. And really, is there a downside to drinking hot cocoa?
The benefits are likely not limited to cocoa powder just because that was the substance observed in this experiment. Raw cacao beans and 70% dark chocolate or higher are rich in the same compounds, minerals like selenium, and anti-oxidants, and can offer the same benefits.
Peppermint Extract
The leaves of peppermint (Mentha piperita L.) were found to decrease the production of inflammatory markers, and demonstrated high anti-viral activity against RSV. Peppermint contains high levels of the antioxidants, phenolic acid, and flavonoids, effective at free radical scavenging.
Another study determined peppermint tea has antiviral, antimicrobial, antitumor activity, and even anti-allergy potential. Analgesic and anesthetic effects in the CNS and PNS along with immune activity were demonstrated in animal model studies. Though there haven’t been clinical trials on peppermint tea in humans yet, there is evidence in the trials done with peppermint oil that suggests relief for GI ailments. That’s a lot of benefit.
Drink peppermint tea, chew peppermint leaves, muddle them, and put them in green tea, or diffuse high-quality peppermint essential oils.
Turmeric/Curcumin
Turmeric is a yellow spice related to ginger common in Asian cuisine, and curcumin is the compound isolated in this beneficial root. It has been studied to find powerful antiviral, antibacterial, and antimicrobial properties, even against HIV, herpes, and hepatitis, as well as the bacterial staph, strep and pseudomonas.
Consider buying the root fresh and adding chunks into a fresh smoothie, or sprinkle the ground version over every meal for a little kick to your palate and immune system. Curcumin is also available in supplement form
Fresh Ginger
Studies show this spicy root is a potent antiviral blocks the viral attachment of HRSV in respiratory tract cell lines. The active compound in ginger, allicin acts as an anti-flu cytokine (immunomodulating agent) It’s benefits are greater when consumed fresh, so along with your turmeric, grab some ginger root and toss it in your smoothie, or steep it in a tea.
Don’t Stop Here
I could go on and on, listing all of the things that can assist the body in its natural defenses and help to heal when illness strikes. Above all else, question everything (even what I’ve written here), do your own research, be your own advocate. There’s certainly a lot of information and misinformation available today, and even good information can be interpreted in many ways. Not all professionals are infallible, and not all research is sound. Trust your gut, and weigh your pros and cons when making health choices, but do make health choices. Take care of you, and trust your intuition about what’s best for you and your family.
Information in this post is for educational purposes only, and is not intended to diagnose or treat any disease or condition. Consult your primary care provider prior to making any changes in your diet or lifestyle habits as discussed.
A very special thanks to NFPT-CPT, Daniel Braun who was gracious enough to share all of his resources and notes on the podcast he recently put out on Immune System Biohacks. He basically did most of the leg work and I filled in the words.
Daniel Braun is an NFPT-CPT and currently in graduate school for his Doctorate of Physical Therapy at Lebanon Valley College. Dan founded Brawn Body Training Holistics, LLC, about a year ago with the goal of providing holistic health and fitness services to help others achieve their goals. Dan enjoys studying anatomy (he spent 6 weeks performing a cadaver anatomy dissection), physiology, biohacks, strength and conditioning, and injury-prevention. In addition to workouts, school, and running his business, Dan enjoys hiking, wakeboarding, downhill skiing, cooking, reading, and helping others achieve their goals.
Haven’t listened to his podcast episode yet? Click here to open the episode in anchor, or click here to get to the podcast channel on Spotify.
References
Campbell Biology, 11th edition (2016). L.A. Urry, S.A. Wasserman.
Pathology: Implications for the Physical Therapist (2014)
http://journal.isv.org.ir/article-1-205-en.pdf
https://www.ncbi.nlm.nih.gov/books/NBK548448/
https://www.ncbi.nlm.nih.gov/pubmed/25635594
https://www.ncbi.nlm.nih.gov/pubmed/29883396
https://www.ncbi.nlm.nih.gov/pubmed/30479762
https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
https://www.ncbi.nlm.nih.gov/pubmed/20689415
https://www.ncbi.nlm.nih.gov/pubmed/27872866
https://www.ncbi.nlm.nih.gov/pubmed/14993078
https://onlinelibrary.wiley.com/doi/abs/10.1002/ptr.1936
https://www.frontiersin.org/articles/10.3389/fmicb.2019.00912/full
https://www.ncbi.nlm.nih.gov/pubmed/23123794
https://genominfo.org/journal/view.php?doi=10.5808/GI.2016.14.3.96
https://psycnet.apa.org/doiLanding?doi=10.1037/0033-2909.130.4.601
https://www.ncbi.nlm.nih.gov/pubmed/32153016
https://www.ncbi.nlm.nih.gov/pubmed/25746935
https://www.ncbi.nlm.nih.gov/pubmed/21677052
https://www.ncbi.nlm.nih.gov/pubmed/10714244
https://www.ncbi.nlm.nih.gov/pubmed/9330293
https://www.webmd.com/vitamins/ai/ingredientmono-954/vitamin-e









