When pain is great enough to impact exercise habits or even activities of daily life, clients may pursue medical interventions and burgeoning therapies to help alleviate or even eradicate their symptoms. Personal trainers who are informed on these topics can help guide their clients in the decision-making process and also be prepared for what to expect if a client undergoes a treatment.
Gray Cook, MSPT, OCS, CSCS, says, “Pain Changes everything.”
I tend to agree…if you or a client have ever suffered from chronic pain, I’m sure you can relate too.
Pain can impact motivation, gait, performance, the stability of a joint, the function of a muscle, and a client’s mood, or mindset.
If you’ve got a client in pain, they may be curious about a treatment called Platelet Rich Plasma, or PRP, or may even be receiving PRP treatment already. They may ask you what it is and what your take on it might be.
What is PRP?
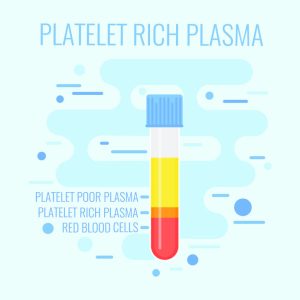
PRP is a substance that comes from your own blood. It’s made up of a concentration of platelet cells that have growth factors (Cluett, 2019).
What are platelets?
Platelets are a vital part of the human immune system. They are small colorless disk-shaped cell fragments. They have no nucleus and are found in large numbers in the blood.
What are growth factors?
Growth factors are chemicals found in the human body that signal it to start the healing process. They are important in the healing process because they play a large role in new tissue construction (Cai et al., 2015).
What is PRP Treatment and how does it work?
PRP treatment is a process that uses the human body’s own healing properties to treat soft tissue injuries such as the ones listed above (i.e.: tendinitis, ligamentous injury (sprains), nerve damage, and osteoarthritis (Bogash, n.d.).
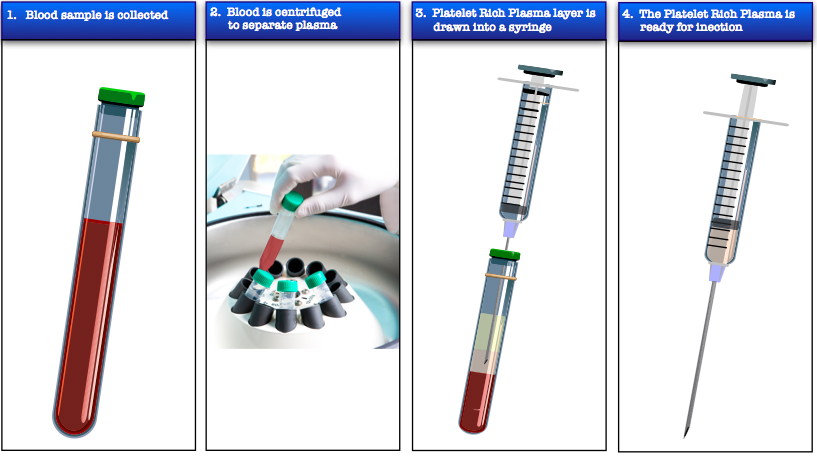
Basically, a person getting PRP can expect to work with a credentialed, licensed medical provider who will do a blood draw. Once the blood is drawn, it is placed in a centrifuge for several minutes. This allows the part of the blood that contains the healing factors (the white blood cells, where the platelets are found) to rise to the top and leaves the reaming parts of the blood (the red blood cells) at the bottom.
The medical provider can then extract the portion of the blood where the healing factors are located and re-inject them into the site of injury or the part of the human body that’s being treated.
It is recommended to discuss how many injections and the length of treatment with the medical provider. This can vary based on the severity of injury and its location.
What PRP is not:
PRP is not the same as a cortisone or steroid injection. PRP comes from your own body and is re-injected into the site of injury with the intention for the human body to use its own healing properties to regenerate and heal, treating the root cause.
Just like any medical or treatment procedure, it is not a quick fix or a guaranteed result. It’s important to follow the medical provider’s instructions after the treatment is done for optimal healing. It can involve some rest after the injections to let the PRP do its work in the joints.
A measure of patience and consistency is needed, but it is showing favorable results and gaining popularity.
This treatment is currently being used to treat pain resulting from the following conditions (Bogash, n.d.):
- Torn or sprained ligaments
- Tendon injuries
- Tennis elbow
- Plantar fasciitis
- Rotator cuff injuries
- A bulging or herniated disc
- Soft tissue damage due to sports or exercising
- Sacroiliac problems
- Sciatica or sciatic nerve pain
- Carpal tunnel syndrome
- Skier’s or “gamekeepers” thumb
- “Texting thumb”
- Chronic pain in a joint
- Joint instability, stiffness, and loss of flexibility or range of motion
From http://ipcpaincenter.com/platelet-rich-plasma-prp/
Regenerative Medicine
PRP treatment falls under the Regenerative Medicine category. Per Alves and Grimalt (2017), PRP was conceptualized in the 1970s by hematologists. Hematologists specialize in the field of hematology, the science or study of blood, blood-diseases, and blood-forming organs. Some diseases treated by hematologists would include hemophilia, leukemia, lymphoma, sickle-cell anemia or thrombocytopenia (low blood platelet count in the human body)..
They coined the term PRP to describe plasma that had a richer platelet count than peripheral blood. Peripheral blood refers to all the cellular parts of blood (red blood cells/erythrocytes, white blood cells/leukocytes, and platelets) found in blood that circulate in the human body.
In the 1980s, PRP started to be utilized in maxillofacial surgery (surgery specializing in the mouth, jaw, and face), in the form of PRF (Platelet Rich Fibrin, another type of platelet concentration). PRF contains fibrin which has adherence potential and hemostatic properties, helping blood to clot and injuries to heal, or in this case, post-surgical healing. PRP, on the other hand, was designed to stimulate cell proliferation and utilized for its anti-inflammatory effect.
Since then, PRP has been used by licensed medical professionals in the musculoskeletal field with sports injuries and other types of soft tissue conditions.
Other fields of medicine where PRP has gained prevalence are:
- Pediatric surgery
- Gynecology
- Cardiac surgery
- Urology
- Ophthalmology
- Plastic surgery
Of late, PRP treatment is gaining traction in dermatology due to its tissue regenerative properties for wound healing, skin rejuvenation, alopecia (an autoimmune disease creating hair loss), and scar revision. Studies show that PRP increases type 1 collagen synthesis and can stimulate human dermal fibroblast proliferation when injected appropriately.
New collagen deposition, new blood vessels, and tissue formation make it useful in the field of dermatology (Alves & Grimalt, 2017).
More on PRP Treatment:
It’s now also been found that platelets contain a vast amount of growth factors and cytokines and can positively impact inflammation, angiogenesis (formation of new blood vessels), cell proliferation, and stem cell migration.
The platelets in PRP are vital and PRP itself serves as a natural source to signal molecules once the platelets in PRP is activated. The key to remember is that PRP contains platelet levels that are above the baseline of platelets contained in peripheral blood of the human body (before they are placed in a centrifuge).
Another key to PRP is that once the blood drawn is placed into a centrifuge, the blood will separate into its parts based on their densities (as in the image below).

From: https://www.khromdermatology.com/prp-face-neck/
PRP that is used for the treatment of musculoskeletal and soft tissue injuries will typically have higher numbers of leukocytes (white blood cells). These healer cells can be activated by PRP kits or other methods to be used along with platelets when they are re-injected into the body. This initiates the healing process.
Who is the ideal candidate for PRP treatment?
PRP treatment is not for everyone. An ideal candidate would have the following characteristics:
- Those who are open to natural treatment methods.
- Those looking for alternatives to orthopedic surgery.
- Those who do not have an acute injury (one that’s recent and needs immediate medical attention).
- Those who are in good general health with an uncompromised immune system (this is important since the PRP comes from your own blood).
- Those who have any of the above-mentioned conditions.
Costs associated with PRP Treatment:
PRP treatment is not yet covered by most insurance plans, therefore there is usually an out-of-pocket cost for it. You can try to go through an appeal process if your insurance policy doesn’t cover it, but since research is currently being conducted on its long-term efficacy, the appeal may not be approved.
Medical practitioners can charge between $500 and $1,000 per injection, and sometimes even up to $2,500. Some medical practices will offer a package program based on how may injections are purchased and needed to adequately treat the impacted areas. It is important to discuss the financial investment up front with the provider. You may also want to do research and when the option is available, talk to other providers in the area to ensure you are receiving a competitive rate.
My Injury and Experience with PRP Therapy
A little more about my story: I had developed tendonosis in my left shoulder and inflammation around the soft tissue in my rotator cuff from playing competitive sports throughout my life. It’s been a persistent issue for over 20 years.
I wish I knew then what I know now, but am amazed that treatments such as these exist. In addition to the recommended approaches like RICE and eventually PT, I had tried other forms of therapy such as:
- prolotherapy
- acupuncture
- cupping
- gua sha
- dry needling
- electric stim
- reiki
- KT Taping
- kinesiology guidance
While all were giving me some relief, none were lasting. I was interested in trying PRP after learning more about it and how it is touted for cell regeneration.
Before the injections were administered, my medical team performed an ultrasound exam so they could determine exactly the best areas in the joint to inject. This is an example of what can take place with a shoulder issue; obviously, PRP can be used for other joints and connective tissue. The shoulder cavity is larger than joints such as the wrist or ankle, so the imaging helped locate the most effective injection sites.
Here’s a video showing the ultrasound exam that was done. Once the ultrasound was done, it was also explained to me where the injections were to be made and why:
I went through three rounds of injections, the first in January 2019. Each subsequent round of injections was done two weeks following the last one, respectively. Research indicates that PRP tends to be more effective over a period of time,
Plus, the fact that my shoulder pain was chronic, played a role in deciding on multiple rounds of injections. If you are considering PRP treatment, it is important to have these important discussions with your treatment team while taking medical considerations into account.
We spread the three rounds of injections over 6 weeks. The first one was January 17, the second one was January 31 and the final injection was February 14. PRP tends to be more effective over a 6-month time frame than short-term (3-6 weeks) corticosteroid injections, with results peaking 6-9 months after the final injection. (Fedato et al., 2019; Lin et al., 2019). Not to mention that corticosteroid injections oftentimes don’t treat the root cause of the issue.
Due to the large region of the shoulder and its three degrees of freedom, my outcome was unfortunately not very favorable. The doctors who performed the procedure informed me that the shoulder is a challenging joint for PRP because the injected treatment (my own platelets) didn’t have a chance to stay within the joint long enough to “work their magic”. Despite resting afterward and limiting movement, the qualities of the shoulder joint make success difficult.
While I don’t feel worse, I don’t feel better either. I don’t fault the doctors since this was a trial and we adhered to current research stating the benefits of PRP therapy.
While PRP is not a new treatment, the use of it in this capacity is relatively new. There is some supporting research that PRP treatment can be beneficial to augment rotator cuff treatment but its use as a stand-alone treatment in rotator cuff tears is inconclusive.
There is very little research on its use in the glenohumeral joint and my specific condition and we must also take into consideration that my injury was long-standing. There is research done on a case study of using PRP to successfully treat tendinitis in a patient, yet the case study used didn’t have the history with her injury that I did.
Despite the lackluster results of the PRP treatment in my shoulder, it was beneficial to try it. The procedure was minimally invasive and the research does support its safety when using it in the adult human population. There is also research supporting PRP’s results in terms of improving pain, disability, and shoulder range of movement in patients with adhesive capsulitis of the shoulder.
An Unexpected Outcome
While I only highlighted my PRP therapy done on my shoulder, I also had an ankle injury that was treated with PRP before I ventured to have the series done on my shoulder. Having suffered a grade 1 inversion ankle sprain of my left lateral collateral ligament complex in 2017 that was successfully treated with physical therapy, corrective exercise, and PRP injections.
I used the same docs for my ankle injury as I did for the shoulder treatment. I talked to them about why the treatment went well for the ankle. They said chiefly that the ankle is a smaller, less mobile joint, so the medication (my PRP) could sit in the joint and do its work longer than in a larger joint such as the shoulder.
Also, the ankle joint (or talocrural joint) is a synovial joint formed by the bones of the leg (fibula and tibula) and the foot (talus). It’s classified as a hinge joint (allowing for dorsiflexion and plantarflexion), thus has fewer degrees of freedom than the shoulder (the ankle joint has two degrees of freedom). Since it has less movement and is a smaller/tighter area, the PRP was able to saturate it more.
The doctors additionally discussed the probability that since the injury was more recent and not a chronic, recurring injury, it may have had better results. Research supports these statements; PRP is an effective treatment for the treatment of acute lateral ankle sprains.
PRP Takeaway
The purpose of this article wasn’t to put PRP on the ‘chopping block’ or put the onus onto my docs or even the therapy for the failed shoulder outcome. The fact is, the PRP worked beautifully on my ankle. Since it had worked so well on the ankle, we tried it on the shoulder, and with fingers crossed, given available research.
Overall, I felt it was worth the investment in money and time despite no improvement in my shoulder. Given my experiences, both noteworthy and disappointing, any fit pro would benefit from being informed on the topic. There are some amazing treatment modalities out there and our clients look to us, inquiring about the latest and greatest all the time.
We can’t draw general conclusions based on my experience alone and make a blanket statement that PRP is not effective in larger regions of the body or ball and socket joints. Obviously, we didn’t try it on my hip joint!
Other factors to consider:
- My ankle injury had been acute and fairly recent, whereas I had struggled with the shoulder injury for years.
- We have discussed doing more injections in the shoulder region or even the stem cell procedure. For now, though, I have yet to make that decision. Perhaps additional treatments will be more effective?
- I’m continuing to do corrective exercise techniques for my shoulder and making sure it stays in optimal positioning during my training so as not to make it worse.
PRP is not for everyone. Sometimes surgery or other treatments are needed. This is a conversation to have with your medical provider and loved ones. I sometimes have clients who are either currently getting PRP treatments or asking me about it. I have personal experience with it that’s been positive and I’m always looking to educate my clients and colleagues using solid sources about what’s available in the industry.
There’s much more to be said about PRP treatment such as its history, current research on the treatment, its long-term effects, and my own experience with the treatment. While the use of PRP for soft-tissue injuries is relatively new, the concept is not. Because of this, much of the presenting research includes case studies and larger clinical trials are pending.
There’s plenty of reading and approaches to take for shoulder issues such as assessing and preparing the shoulder for pull-ups and strengthening it. Don’t forget proper warm-up techniques for the shoulder before starting a training session is the best way to improve mobility and prevent injury.
References
www.leeds.ac.uk/chb/lectures/anatomy4.html
Seijas, R., Ares, O., Alvarez, P., Cusco, X., Garcia-Balletbo, M. & Cugat, R. (2012). Platelet-rich plasma for calcific tendinitis of the shoulder: A case report. Journal of Orthopaedic Surgery, 20(1), 126-30.
Alves, R. & Grimalt, R. (2017). A review of platelet-rich plasma: History, biology, mechanism of action, and classification. Skin Appendage Disorders, 4, 18-24. DOI: 10.1159/000477353
Barber, F. A. (2018). PRP as an Adjunct to Rotator Cuff Tendon Repair. Sports Medicine & Arthroscopy Review, 26(2), 42-48.
Barman, A., Mukherjee, S., Sahoo, J. Maiti, R., Rao, P.B., Sinha, M.,….& Bag, N.D. (2019). Single intra-articular platelet-rich plasma versus corticosteroid injections in the treatment of adhesive capsulitis of the shoulder: A cohort study. American Journal of Physical Medicine & Rehabilitation, 98(7), 549-558.
Biel, A. ( 2015). Trail Guide to Movement: Building the Body in Motion. Books of Discovery: Boulder, CO.
Blanco-Rivera, J., Elizondo-Rodríguez, J., Simental-Mendía, M., Vilchez-Cavazos, F., Peña-Martínez, V., & Acosta-Olivo, C. (2018). Treatment of lateral ankle sprain with platelet-rich plasma: A randomized clinical study. Foot and Ankle Surgery (2019).
Bogash, J. (n.d.). PRP Therapy. Retrieved from: https://www.lifecarechiropractic.com/prp-therapy-mesa-az/
Cluett, J. (2019). Platelet-rich plasma (PRP) Injection: Natural injections to heal damage and reduce inflammation. Retrieved from: https://www.verywellhealth.com/platelet-rich-plasma-prp-injections-2549576
Cook, G. (2010). Movement functional movement systems: Screening, assessment, corrective strategies. Santa Cruz, CA: On Target Publications.
Ebert, J. R., Wang, A., Smith, A., Nairn, R., Breidahl, W., Zheng, M.H., & Ackland, T., (2018). A midterm evaluation of postoperative platelet-rich plasma injections on arthroscopic supraspinatus repair: A randomized controlled trial. American Journal of Sports Medicine 46(13), 2965-2975.
Fedato, R. A., Francisco, J. C., Sliva, G., de Noronha, L., Olandoski, M., Faria, J. R., Ferreira, P. E.,….Gaurita-Souza, L. C. (2019). Stem cells and platelet-rich plasma enhance the healing process of tendinitis in mice. Stem Cells International, Article ID 1497898, 1-9. https://doi.org/10.1155/2019/1497898
Lin, M. T.., Chiang, C.F., Wu, C. H., Huang, Y. T., Tu, Y.K., & Wang, T.G. (2019). Comparative effectiveness of injection therapies in rotator cuff tendinopathy: A systematic review, pairwise and network meta-analysis of randomized controlled trials. Archives of Physical Medicine and Rehabilitation, 100(2), 336-349. https://doi.org/10.1016/j.apmr.2018.06.028
ShayTheCoach. (2019, May 14). STC LifeCare PRP Explained. Retrieved from: https://www.youtube.com/watch?v=fyjhTShQEKU
ShayTheCoach. (2019, May 14). Platelet Rich Plasma – The Details and The Uses – ShayTheCoach and LifeCare Chiropractic.
Retrieved from: https://www.youtube.com/watch?v=cqboLcbN0Hs&feature=youtu.be
ShayTheCoach. (2019, May 22). Platelet Rich Plasma – Why ShayTheCoach Was A Candidate. Retrieved from: https://www.youtube.com/watch?v=fcON8adrSL8&t=77s
Shaweta “Shay” Vasudeva, MA (Psychology), MS (Kinesiology), NFPT-CPT, NASM-CPT-CES, THSA-CNT, and Tai Chi & Black Belt Karate Instructor is a teaching professional, speaker, author, coach, and cat lover! Her passion is to help people become the best version of themselves by using an interdisciplinary and holistic approach, bringing 10+ years of experience in Psychology, Personal Fitness Training, Corrective Exercise, Nutritional Coaching, Cranial Sacral Work, and teaching Karate & Tai Chi classes to her business, ShayTheCoach. Shay teaches classes at Maricopa Community College District as an Adjunct Professor. For more information visit her personal webpage: www.shaythecoach.com

