Coaching clients with chronic illnesses requires more than simply writing fitness programs or offering health coaching. It requires a level of dedication that encompasses compassion, adaptability, and a recognition/ understanding of their unique challenges. In this article, we will delve into ways that trainers, through physical exercise, can support clients and build self-efficacy, resilience, and emotional fortitude. By doing so, we can help these individuals create a more empowering road to wellness.
Defining Chronic Illness
Chronic illnesses fall under a very broad umbrella, encompassing various long-term health conditions. Often, clients who come to us suffer from 3 or 4 comorbidities, further complicating their situations. Each condition will pose its own unique challenges. The examples listed below help to illustrate the diversity as well as the impact of these conditions:
- Diabetes: a metabolic disorder characterized by high blood sugar levels over a prolonged period; requires ongoing management of lifestyle/diet/medication
- Heart Disease/Chronic Respiratory Disease: encompasses conditions such as congestive heart failure, coronary artery disease, and COPD; often involves long-term management through medication, lifestyle changes, and sometimes surgery
- Chronic Kidney Disease: gradually losing kidney function over time, patients can expect this condition to lead to hypertension, anemia, and nerve damage. Chronic kidney disease requires ongoing management/monitoring, medication, and lifestyle/nutritional changes
- Autoimmune Diseases: the body’s immune system attacks its tissues, leading to chronic inflammation and other symptoms
- Cancer: marked by abnormal cell growth affecting different parts of the body, treatment often includes surgery/chemotherapy/radiation/managing side effects
- Neurological Disorders: examples include multiple sclerosis and Parkinson’s disease, which affect the nervous system and require complex, ongoing treatment/management
- Mental Health Disorders: emotional conditions such as anxiety/depression/OCD/eating disorders, which require continuous care/management, often involving therapy and medication
- Chronic Pain: conditions like fibromyalgia and neuropathic pain, which often cause long-term discomfort in the absence of a specified diagnosis. Managing chronic pain typically involves a unique combination of medication/physical therapy/lifestyle modifications
Living with a chronic illness extends beyond managing physical symptoms; it profoundly impacts emotional and psychological well-being. Recognizing and addressing the emotional impact through emotional support, therapy, and self-care strategies are crucial. Personal trainers can aid individuals in coping effectively, improving their quality of life while managing their chronic condition.
Hope for a Pervasive Situation
Chronic diseases top the list of morbidity and mortality in Europe, accounting for more than 66% of all deaths and 75 % of the healthcare costs. In this country, almost 50% of Americans find themselves affected by chronic illnesses, making this a widespread occurrence.
The increasing prevalence of chronic diseases, paired with their enormous economic burden as well as the dramatic shortage of healthcare providers, poses a critical threat. Many attempts to solve these problems have failed, and professionals now recognize the need for a new approach.
Therapist Famous Erwin, LMHC, LPC, MA, a therapist who works with clients living chronically ill clients, shares these thoughts: “Implementing strategies such as social support networks and coping mechanisms significantly aids in stress reduction, pain management, and enhancing overall quality of life. These practices, essential to managing chronic illness, involve developing a comprehensive plan of action to address various aspects of life affected by the condition. By actively managing elements such as diet, exercise, and emotional well-being, individuals can better face the challenges of illness and empower themselves to navigate their health journey more effectively. Through promoting a supportive environment and embracing proactive approaches, individuals can enhance their resilience and improve their overall well-being despite the presence of chronic illness.”
Helping within Our Scope of Practice
Upon first receiving a diagnosis of chronic illness, most individuals find themselves faced with the pressing need to consider things like symptom management, medication, potential physical limitations, uncertainty/fear, and, most importantly, the impact this illness will undoubtedly have on overall quality of life. In the wake of these challenges, mental health issues begin to surface.
Clearly, helping clients cope with a chronic illness requires a multifaceted approach, addressing social, mental, and physical well-being. While personal trainers cannot legally attend to the medical needs of such clients and must likewise tread lightly when it comes to nutrition suggestions, we can make more of a difference than previously understood. Today’s medical professionals emphasize patient responsibility, having discovered that self-management might represent a promising strategy. By teaching individuals to actively identify challenges, they can then seek out community resources, for which personal trainers do qualify.
Maintaining healthy lifestyle habits, or walking through dramatic lifestyle changes often necessitates significant support. Personal trainers can make a profound difference for a client’s overall physical and mental wellness; this regular physical activity can release endorphins and boost mood.
The Holistic Approach
Chronic illness, at first an overwhelming experience, often elicits feelings of helplessness and frustration. Chronic diseases prove challenging to cope with for a variety of reasons; most importantly, many patients find it difficult/embarrassing to have to ask for help and support from friends and family members. Prior to their health situation, most of these individuals had easily accomplished basic tasks by themselves, such as cooking, cleaning, and bathing/dressing. Just the uncertainty of the rest of their lives often invokes fear, which only serves to exacerbate mental health.
Many recently diagnosed individuals may not realize that they can find support within the fitness world. A personal trainer can make a significant impact on someone’s life, yielding benefits beyond simply improvements in strength and body composition. Through proper and medically approved exercises, we can reduce stress, mitigate feelings of isolation/loneliness/depression, and offer uplifting encouragement.
Knowing the Right Words
When a client living with a chronic illness expresses feelings of sadness, anger, embarrassment, or helplessness, personal trainers must learn to respond appropriately. Refrain from trying to minimize the situation; this only leads to a person feeling shame or guilt. Instead, we can choose some more empathic and helpful phrases, such as ~
- “Wow, that sounds difficult to deal with.”
- “I can’t imagine how this feels, but I’m here for you.”
- “That sounds frustrating—I am ready to help.”
- “I am listening.”
- “I want to safely support you however I can.”
Clients will present with different co-existing chronic conditions and complications, all of which personal trainers need to understand before establishing a successful partnership. In addition, we must take into account the individual’s social, financial, and psychological “comfort zone” prior to training. By listening to a prospective new client’s views on all of the above, trainers can strive to formulate a mutually agreed-upon, realistic set of goals.
Structural, Functional, and Metabolic Considerations
Often the manifestation of a client’s symptoms falls into 1 of 4 categories: structural complications, functional, psychosocial, and/or metabolic issues. Many will exhibit comorbidities. Prior to embarking on training, establishing a baseline for where the client’s comfort level rests with regard to these issues will go a long way towards building trust.
The structural category represents the physical components that affect the client. Chronic illness often has to do with constant pain, which will naturally play a dominant role in how a personal trainer designs the workout.
When a trainer addresses function, the inquiry should relate to determining if the client’s muscles/joints move properly; can he use his body to its full potential in terms of range of motion?
Sometimes chronic pain comes on as a result of eating certain foods or particular environmental exposures; these issues fall under the metabolic category. Conditions such as diabetes, autoimmune diseases and celiac disease can compromise the body’s ability to heal properly. A trainer must take these into consideration as well.
Stress
While the aforementioned 3 categories address the physical aspects of a chronic illness, psychosocial issues reflect the non-physical, or the contribution of social and mental wellness to a person’s chronic pain.
In the context of daily discomfort, trainers need to consider whether stress directly aligns with the onset of a client’s symptoms, as well as how it might impact on the individual’s ability to recover properly between training sessions. Understandably, few if any people living with a chronic illness report zero stress in their lives. This value may also change from day to day.
The Importance of Pacing
Pacing, a tried-and-true pain management technique, can help both trainer and client learn to balance activity and rest while still working towards goals. This certainly requires practice, especially in the case of chronically ill patients previously accustomed to a more physical lifestyle. Below we present some tips for mastering the art of pacing ~
- Learn to recognize signs of fatigue or pain
- Avoid overexertion
- Break big tasks into smaller, more manageable ones
- Schedule rest periods between sessions
- Use timers or activity trackers to help monitor the client’s energy level
- Adjust as needed
The Holistic Approach
Both medical and fitness professionals have found that, when working with chronically ill individuals, introducing the concepts of holistic wellness practices into these patients’/clients’ daily routines can significantly enhance their quality of life. Given the individual’s unique physical status, personal trainers may choose to consider the following ~
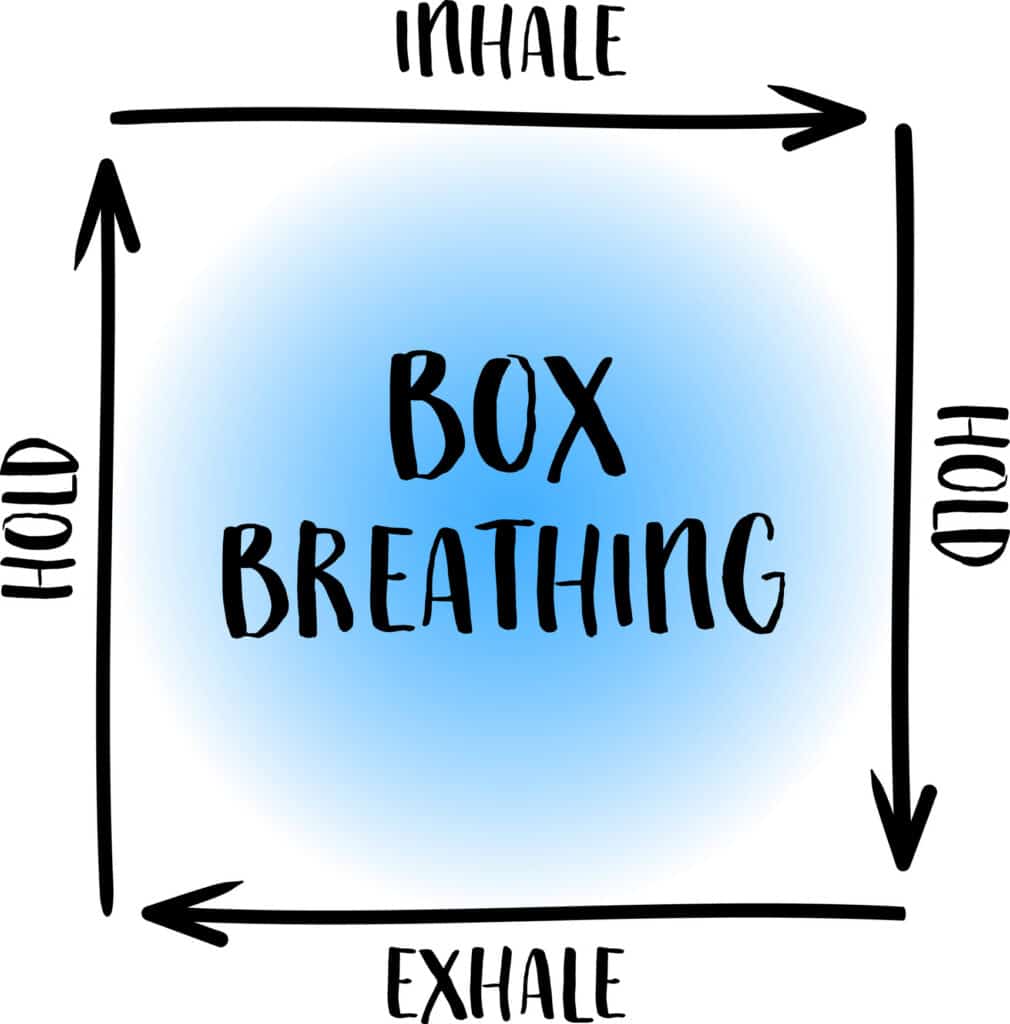
- Mindfulness/Yoga: poses and breathing techniques help manage stress and pain associated with chronic conditions; increase “living in the moment” awareness and relaxation, helpful for the emotional challenges of chronic illness
- Nutrition: suggesting nutritional counseling can help patients make specific choices that can help mitigate symptoms
- Personalizing Goals: by helping these individuals customize wellness routines that align with their unique needs — as we would for any client — we can improve their lifestyle; focus lies on attainable goals, an appropriate level of exertion, and workouts that cultivate empowerment and self-efficacy
What Personal Trainers Can Learn from the Medical Model
A patient’s first line of care begins with his medical team, experts in the field of addressing chronic illnesses. Fitness professionals serve as an adjunct to traditional treatment. Though our approach differs somewhat, many of the positive aspects of the medical model can indeed translate into the personal training world.
Living with a chronic illness means adapting to an ever-evolving process of balancing disease-related symptoms with everyday tasks at home, work, and in regard to recreational endeavors. While the primary job of healthcare professionals involves medical support and symptom management, another key aspect of said support involves educating individuals with chronic conditions on how they can actively participate in their own care.
Studies of the approach taken by primary care nurses revealed the importance of promoting self-management for the patient. Emphasizing patient autonomy and refraining from seeing symptoms as limitations helps them focus on their ability to live a positive “new normal” lifestyle. The nurses in the study emphasized the need to familiarize themselves with their clients’ social environments/lifestyle preferences to more optimally offer recommendations for dealing with the manifestations of their diseases.
Resilience and Self-Management
Resilience plays a huge role in acquiescing to the self-management responsibilities of chronic illnesses. By understanding the science behind resilience, the complexity of psychological, biological, and social aspects, personal trainers can design more targeted exercise protocols to support their clients.
The human brain boasts the uncanny ability to rewire itself through a process known as neuroplasticity, defined as the ability of the nervous system to change its activity by reorganizing its structure, functions, or connections following any trauma. Chronic illness may induce such trauma; fortunately, resilience can strengthen over time. Appropriately chosen personal training exercises, like the more cognitive practices of mindfulness and meditation, can physically reshape neural pathways to enhance adaptive mechanisms.
Final Thoughts
When working with a chronically ill client, personal trainers must recognize that what we offer transcends pure body mechanics. We hold the power to shift an individual’s perspective, reframing a negative mindset into a more hopeful, optimistic outlook. We can foster self-efficacy, the belief in one’s ability to overcome stumbling blocks and find solutions for navigating adversity. We help these individuals manage their emotions by enabling them to move more successfully through daily activities, thereby averting or at least minimizing overwhelming distress.
As previously mentioned, we can learn much about our interactions by incorporating and mastering proven techniques from the medical model: a warm and caring approach, superior listening skills, and ultimately heightening a client’s social connection with the world.
References
https://www.willowshealthcare.com/blog/how-to-address-the-emotional-impact-of-chronic-illness
https://my.clevelandclinic.org/health/articles/4062-chronic-illness
https://pmc.ncbi.nlm.nih.gov/articles/PMC9008851/
https://pmc.ncbi.nlm.nih.gov/articles/PMC3042340/
https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-015-2303-3
https://onlinelibrary.wiley.com/doi/10.1111/jocn.12827
https://bmcprimcare.biomedcentral.com/articles/10.1186/s12875-022-01687-x
https://www.aafp.org/pubs/fpm/issues/2010/0900/p24.html
https://pmc.ncbi.nlm.nih.gov/articles/PMC4103232/
https://www.ncbi.nlm.nih.gov/books/NBK557811/