As fitness professionals, we often hear complaints from clients about various muscle aches following tough workouts. Typically we can dispel their fears by explaining the principle of DOMS (Delayed-Onset Muscle Soreness), and reassure them that they truly can work through the pain without evoking further damage. The most commonly reported sites of post-workout pain are the lats, pectorals, and quads. However, occasionally we are faced with a client who has unexplainable pain deep in the gluteals, often accompanied by radiating pain down one leg.
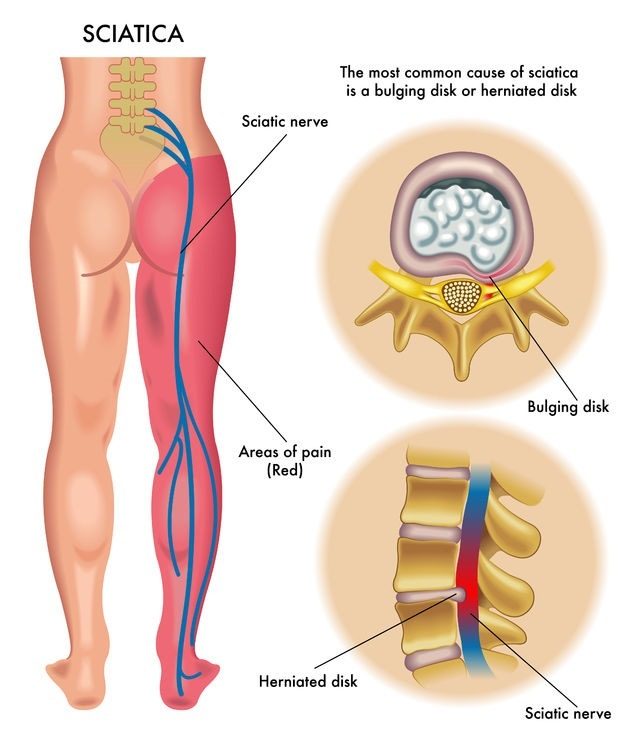
In the absence of any easily explainable recent acute trauma to that particular area, the client may be experiencing the less common but extremely painful condition known as Piriformis Syndrome. Piriformis Syndrome is a neuromuscular disorder that occurs when the sciatic nerve is compressed or otherwise irritated by the piriformis muscle. The result of this compression is pain, tingling and numbness in the buttocks; continuing along the path of the sciatic nerve, these sensations descend down the lower thigh and into the leg and foot. While diagnosis of this disorder proves challenging due to the lack of accurate tests, a highly telling criterion is eliminating the possibility of Sciatica resulting from compression of nerve roots, as is seen with herniated discs.
The piriformis muscle is flat, pyramid-shaped, and oblique. This muscle originates in a position anterior to the S2-S4 vertebrae, the sacrotuberous ligament, and the upper margin of the greater sciatic foramen. As the piriformis passes through the greater sciatic notch, the muscle inserts on the superior surface of the greater trochanter of the femur. When one’s hip is extended, the piriformis muscle is the primary external rotator; however, during hip flexion, the piriformis internally rotates, thereby becoming a hip abductor.
When the piriformis muscle shortens or spasms due to trauma or overuse, it begins to compress or strangle the sci
atic nerve, which lies beneath the muscle. Sometimes the symptoms of Piriformis Syndrome may occur as a result of local inflammation brought on by the muscular compression of smaller nerves and vessels-including the pudendal nerve and blood vessels, which exit at the medial inferior border of the piriformis muscle. Regardless of the cause, the end result is pain which can run the gamut from significant to debilitating. The most common presenting symptom is increasing pain after sitting for longer than 15 to 20 minutes. Symptoms may be of sudden onset, or may develop gradually over time, building in intensity, as is seen when the cause is overuse. Typically, patients complain of difficulty walking, and report pain associated with internal rotation of the leg experiencing the pain, such as occurs during sitting in a cross-legged position.
Medical journals describe two separate and distinct types of Piriformis Syndrome. Secondary Piriformis Syndrome accounts for approximately 85% of all cases, originating from causes outlined above: overuse, prolonged sitting, or an actual trauma at the site of the muscle. In a rarer 15% of cases, Primary Piriformis Syndrome results from an anatomic anomaly. In these instances, the sciatic nerve may pierce the piriformis muscle, or the nerve itself may split, with one branch going through the muscle and the other branch passing above or below the muscle.
Piriformis Syndrome is most frequently reported during the fourth and fifth decades of life. It is interesting to note that this condition is more commonly observed in women than men, possibly because of the biomechanics associated with a female’s wider quadriceps femoris muscle angle, also known as the “Q angle” of the pelvis. In addition, as typical primary caregivers, a woman may spend a great deal of time standing and shifting her weight from one foot to the other while holding a baby on one hip. Over time, this repeated movement can cause a change in how core stabilizers are used, and can lead to muscular imbalances and postural dysfunction. In many cases, it is this very dysfunction that will lead to Piriformis Syndrome. Some of the more common biomechanical misalignments associated with the condition are:
- tight hip external rotators
- tight hip adductors
- weak hip abductors
- sacroiliac joint hypomobility
These functional issues, along with the weight-shifting referenced above, can lead to a shortened stride length when walking, and a gait with an externally rotated thigh, both of which have the preponderance of leading to the onset of Piriformis Syndrome.
Once a diagnosis has been ascertained, treatments can vary widely, depending not only upon the direct cause of the syndrome but also upon the intensity of the pain. Some of the more holistic remedies include stretching, ice, deep tissue massage, myofascial release, electrical stimulation, and chiropractic adjustments. In addition, muscle strengthening exercises, working on the hip abductors, external rotators and extensors, can often provide relief.
A prudent strength program should begin with non-weight bearing exercises, to focus on isolated muscle recruitment. Once stabilization is sufficient, weight-bearing exercises may be introduced. Certainly more aggressive forms of treatment may be considered, if these courses of action do not provide relief. Seeking the advice of a properly trained physician is always advisable.
While Piriformis Syndrome is a painful inconvenience, it tends to be one of the more curable neurological disorders. Patience is a must when dealing with the recovery process, as it is easy to exacerbate the condition if not allowed to heal fully. This “pain in the butt” sometimes serves as a chronic reminder to keep our bodies in proper alignment at all times. With a careful eye on our clients during their training, we might be able to observe and correct misalignments before they lead to problems.
References
1. http://en.wikipedia.org/wiki/Piriformis_syndrome
2. http://www.webmd.com/pain-management/guide/piriformis-syndrome-causes-symptoms-treatments
3. http://www.jaoa.org
4. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1317145/
5. http://emedicine.medscape.com/article/308798-overview#a0104
6. http://www.losethebackpain.com/conditions/piriformis-syndrome/

