The cardiovascular system is foundational to exercise, and our understanding as personal trainers of how it works and how things can go wrong is critical for the performance, success, and safety of our clients. Consultation with a medical professional and a physical is recommended to our clients before they start an exercise program to uncover the health status of the cardiovascular system (CVS) and whether it will be adversely impacted by exercise.
Is this enough?
Prioritizing and investigating clients’ health history according to recent research and recommendations to minimize risk and identify potential unknown risk factors is part of the role of a personal trainer. Properly assessing cardiovascular risk becomes a priority when so much of what you do with your clients can impact the cardiovascular system.
As with any physical activity, there’s a risk of injury or – in very rare cases – a catastrophic outcome.
Here’s what you need to know when gathering critical health information.
Pre-participation Health-Screening Guidelines
In November 2015, The American College of Sports Medicine (ACSM) updated the pre-participation health-screening guidelines in an effort to remove excessive medical barriers to participating in physical activity.
While the previous CVD risk factor algorithm was thorough, it was also complicated and left fitness professionals frequently making an unwarranted number of referrals clients to physicians for medical clearance. Research has questioned the effectiveness of the former screening tool.
A study by Whitfield, Gabriel, Rahbar, and Kohl (2014) suggested that greater than 90% of adults 40 years old and older would receive a recommendation for physician clearance prior to beginning any exercise regimen. That’s a staggering number of clients who want to be active only to become derailed or discouraged by a potentially unnecessary extra step.
Consequently, this created excessive medical barriers for clients (Whitfield, Riebe, Magal, & Liguori, 2017). To remedy this issue, a new algorithm was developed. Initial research results demonstrated that the number of individuals who would, under the previous guidelines, be referred to a physician for clearance decreased by 41% with the new guidelines (ACSM, 2018).
Another great benefit of the new screening approach is that it places more responsibility upon the medical professional to decide who needs what type of test and why thus taking the guesswork out of screening by personal trainers. All the exercise professional needs to do is use the updated algorithm and make the referral for medical clearance where necessary. Features of the new screening tool:
Features of the New Screening Tool
According to research, the new tool and the need for medical clearance prior to beginning an exercise program is based on the following variables.
- An individual’s current exercise participation
- History of cardiovascular, metabolic or renal disease or signs or symptoms suggestive of disease
- Desired exercise intensity of the client
(Riebe, Franklin, Thompson, Garber, Whitfield, Magal, & Prescatello, 2015).
The first step in using the new tool is to identify those individuals who do or do not participate currently in exercise. The goal is to more accurately and clearly classify individuals who are simply unaccustomed to activity from those who may legitimately be at risk for cardiac complications.
Next, depending on the category (currently active or inactive), personal trainers will use one of two flow charts. There are three categories on each chart for the two classifications of individuals. Each category is detailed in the charts and directs the trainer to proceed accordingly.
View the Chart from ACSM in this article – Figure One
For example, if a client who does not participate in regular exercise and has known cardiovascular, metabolic, or renal disease AND is asymptomatic (the second category under the “does not participate in regular exercise” classification), medical clearance is recommended.
Then, following medical clearance, the client can participate in light to moderate-intensity exercise. The client can progress as tolerated using the ACSM guidelines.
A second example: If a client who does participate in regular exercise and has known cardiovascular, metabolic, or renal disease AND is asymptomatic (the second category under the “does participate in regular exercise” classification), medical clearance for moderate intensity exercise is not necessary.
However, there is a caveat for vigorous exercise. Medical clearance (within the last 12 months if no change in signs/symptoms) is recommended before engaging in vigorous-intensity activity.
Personal trainers should review and learn how to apply the newly developed guidelines and algorithm with their clients. It’s also important for trainers to continue to monitor their clients for any changes that may affect the client’s original classification. Signs and symptoms may develop and would, therefore, require a more aggressive analysis of risk by a qualified medical professional. Consult ACSM’s Guidelines for Exercise Testing and Prescription (10thedition).
Signs and Symptoms of Disease
According to ACSM, major signs, and symptoms that suggest possible cardiovascular, metabolic, and renal disease include:
· Pain or discomfort in the chest, neck, jaw, arms, or other areas that may result from ischemia
· Shortness of breath at rest or upon mild exertion
· Dizziness or syncope
· Orthopnea or paroxysmal nocturnal dyspnea
· Ankle edema
· Palpitations or tachycardia
· Intermittent claudication
· Known heart murmur
· Unusual fatigue or shortness of breath with usual activities
If a client displays or develops any of the above signs or symptoms, refer him or her to a qualified medical professional.
Self-guided Screening
In addition to the systematic process in place for determining a need for medical clearance, any individual wanting to start an exercise program can use the newly updated PAR-Q+ form. This version now includes multiple follow-up questions to better inform preparticipation decisions and risk.
Personal trainers can and are encouraged to use this tool as a supplement to other screening forms and protocols (ACSM, 2018). When it comes to client health history and current physical status, the more information the better.
A substantial body of research indicates the benefits of participating in regular physical activity far outweigh the potential risks. Fitness professionals who thoroughly comprehend and evaluate a client’s risk factors serve to further enhance the known benefits of living an active lifestyle.
Covert Cardiovascular Culprits
Health physicals may miss CVS heritable conditions to include:
- Hypertrophic Cardiomyopathy (HCM) where the walls of the heart muscle thicken causing disruption of the heart’s electrical system, leading to fast or irregular heart beats (arrhythmias)
- Congenital coronary artery abnormalities that are abnormally connected. When the individual with this condition exercises the arteries become compressed decreasing proper blood flow to the heart
- Long QT syndrome–a heart rhythm disorder causing fast chaotic heartbeats often leading to fainting and having increased risk of sudden death. (this can also be induced as a side-effect of medication)
Sudden death of an athlete may be related to any of the aforementioned heritable CVS conditions if not detected prior to engaging in competitive sports. While the condition of HCM can be controlled by surgical implant of a cardioverter-defibrillator, the aforementioned heritable conditions come with the physician’s advice to avoid competitive sports.
Artery Physiology
The endothelium is a single layer of cells that line the inside of the artery. Dr. Michael Greger, MD likens the endothelial cell layer to being the Teflon of the arterial wall, allowing blood/cells to move smoothly. The artery wall has three layers:
- the inner layer (intima): the endothelium that lines the lumen of the vessel
- middle layer (media): the smooth muscle cells and elastic fibers
- outer layer (adventitia) comprised of collagen fibers.
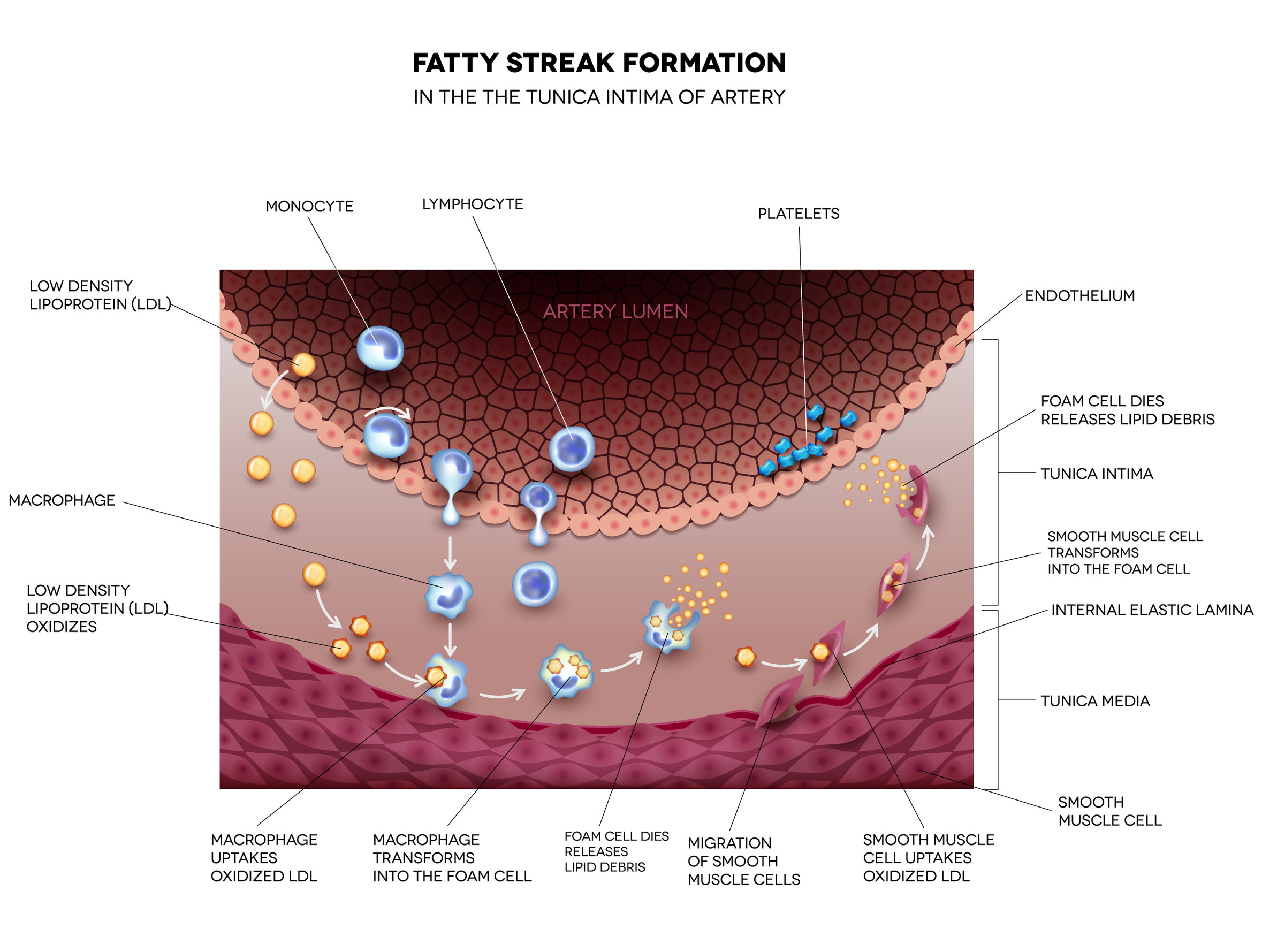
Fatty streak formation in the artery. It may lead to thrombosis, formation of a blood clot inside artery. Copyright: guniita
Cardiovascular Disease/Arterial Plaque
The food we eat directly correlates to the progression of fat streaks in the arteries which are reported to develop as early as the age of 10. These fatty streaks become plaque, a fatty wax-like substance that accumulates over time within the artery wall. As the “bad” cholesterol (LDL) deposits on the arterial wall, macrophages come to ingest the LDL forming foam cells.
The macrophages laden with LDL appear under the microscope as foam-like structures. Foam cells contribute to atherosclerosis by progressing to plaque, which over time becomes unstable, i.e. ruptures the lining of the artery wall. Plaque progression within the wall of the artery causes the intima surface of the artery to bulge into the lumen (the hollow of the artery).
The plaque is composed of lipids, cell debris, smooth muscle cells, collagen, calcium and appears as a white/yellowish bulge within the wall of the artery. Calcification can occur in the intima or media layers of the arterial wall. As plaque grows it will break through the surface causing the body to respond by forming a blood clot. If the clot breaks away it becomes stuck in the artery that feeds the brain or heart and leads to either a stroke or heart attack, respectively.
According to William C. Roberts, editor of the American Journal of Cardiology, the one critical risk factor for atherosclerotic plaque is low-density-lipoproteins (LDL). He suggests removing processed food as well as animal and dairy products to reduce LDL. Likewise, excess white sugar is detrimental causing advanced glycation end (AGE) products that cause cellular damage leading to diabetes, heart disease, kidney failure, Alzheimer’s, all leading to premature aging. Specifically, AGEs will cause oxidative stress and chronic inflammation to our arteries.
AGEs are the covalent attachments of sugars to proteins or lipids. Noteworthy, regarding plaque and its potential to rupture is inflammation caused within the body by processed food, sugar and trans fats, lending to the recommendation of a Mediterranean Diet.
Detecting Narrowing of the Arteries
A CT Scan of the heart and/or MR/PET (Magnetic Resonance/Positron Emission Tomography) scanning can detect artery dysfunction. The MR/PET has lower radiation exposure.
William Fallon says in Life Extension issue Oct 2005: “Many doctors consider radiation from medical X-Rays to be harmless. However, a new National Academy of Sciences report confirms what Life Extension has long argued: that any amount of radiation has a potential to damage DNA, increasing the risk off certain cancer and atherosclerosis.” Further, in the same publication is information from John W. Gofman, MD, PhD, professor Emeritus of Molecular and Cell Biology at Univ. of California, Berkeley. Dr. Gofman notes: “radiation damages DNA in the arteries. The radiation-induced changes create a cancer-like phenomenon in the arteries known as atheroma. Dr. Gofman believes the integration between atheroma and lipids blocks arteries and causes blood clots.”
What can be done?
The gravity of cardiovascular health cannot be understated with both fitness clientele and our general population. If lifestyle factors are not addressed, the development of plaque in the arteries increases the risk of heart events. There are two schools of thought regarding the potential for arterial plaque, or artherosclerosis, can be reversed:
- the first asserts it can only be stalled out
- the other contends that plaque formation can indeed be reversed.
Share these two opposing camps with your clients that are at high risk for or diagnosed with any form of heart disease so they may discuss with the care provider, noting that fatty streaks in the arteries can start as early as age 10; by the age of 35 coronary artery disease develops due to atherosclerosis1.
There is no shortage of articles that can be accessed via PubMed under the topic of atherosclerosis. Key authors that provide highlights from their research are cited below for convenience of comparison. In effect, you will be able to decide whether the only way to prevent plaque progression, once formed, is with statin drugs; or, whether the plaque formation can be reversed by using
Camp 1: Plaque Progression Can Be Halted, Not Reversed
Dr. Howard Weintraub, a cardiologist at NYC Langone Medical Center notes that atherosclerosis is evident in individuals with hypertension, diabetes, and high cholesterol. This collection of conditions is consistent with what is known as Syndrome-X (obesity, hypertension, and high LDL).
His studies purport that the most one can do is prevent plaque progression, i.e. stop plaque from growing. He notes dietary changes can be used to prevent atherosclerosis from getting worse. He also posits that plaque reversal cannot occur. His position includes statin drugs to lower LDL which he believes will prevent plaque from growing. His protocol also includes exercise and diet to reduce hypertension and high cholesterol.
Adding to Dr. Weintraub’s information that was reviewed by Dr. Payal Kohl, MD, FACC is Rena Goldman’s2 information on dietary changes needed to prevent atherosclerosis to include:
- decrease sugar intake
- eat more fiber
- eat healthy fats
- eat leaner cuts of meat
- avoid trans fats
- limit saturated fats
- limit sodium intake
- limit alcohol intake
While all excellent practices to improve overall health, the suggested lifestyle changes are not believed to reverse plaque already formed in the arteries. Rather these lifestyle changes are used to prevent progression of plaque growth. In effect, Dr. Weintraub asserts that arterial plaque requires the use of statin drugs in addition to these changes to halt progression.
Camp 2: Plaque Can Be Reversed
Dr. Michael Greger, MD believes that the body moves forward in the spectrum toward health when provided the opportunity, i.e. the body has an innate direction to heal itself given the correct conditions.
The following resources can be studied in developing one’s own decision of plaque reversal.
(1) Hibiscus Tea vs. Plant-Based diets for Hypertension. (Additional resources by Dr. Michael Greger)
(2) The Cardiovascular Cure. John P. Cooke, MD, PhD.
(3) No More Heart Disease. Dr. Louis J. Ignarro.
(4) The Arginine Solution. Robert Fried, PhD, Woodson C. Merrell, MD.
The aforementioned books and NutritionFacts are summed up by Dr. Jay Wilkins, ND in his YouTube presentation: Nitric Oxide Your Body’s Best Medicine. In his presentation, he concludes that plaque can be reversed.
One pivotal study was done by Dr. Louis J. Ignarro, MD and Dr. Cooke, MD (Head of Cardiovascular research at Stanford) which demonstrated plaque reversal in control rabbits fed a high cholesterol diet with the addition of arginine and citrulline, the amino acids necessary for nitric oxide formation.
Path Forward
To prevent cardiovascular disease exercise plays a part in reversal of arterial damage which primarily becomes causative based on our lifestyle and what we eat. Habits such as smoking, eating processed foods, and sugars will cause fatty streaks in the arterial wall and damage.
The amino acids L-Arginine and citrulline are precursors to nitric oxide that relax the artery and reverse arterial plaque. The following supplements have also been professed to affect LDL cholesterol, promote HDL, and/or relax the artery:
- Nettle cleans cholesterol stagnation. Nettle molecules knock down plaques from the walls of blood vessels, like tiles from walls during repairs. But cholesterol still remains in the blood vessels; it can not move on its own. That is why the second stage is needed.
- Nettle is complimented by Hawthorn extract molecules. Hawthorn – a plant of the rose family – captures the “broken” cholesterol molecules caused by nettles and together they turn cholesterol into useful lipoproteins. These newly formed proteins remove cholesterol from the blood vessels. At this point, fat is burned and energy is released – you feel a surge of strength, health improves.
- Vitamin B1, Thiamine finds blood clots and dissolves them. The remaining calcium is swept away from the walls of blood vessels and no longer threatens to injure veins, arteries and capillaries. The risk of a heart attack drops to zero. Thiamine was shown to have a statistical significant reduction in thrombosis. [Critical Care. 25. Article number:223 (2021). Khalid Al Sulaiman, et.al.].
- Vitamin B2 has a calming effect on the walls of blood vessels. Those that were compressed without normal blood flow return safely and smoothly to normal. Headaches disappear, the tinnitus subsides, the lungs and bronchial tubes work perfectly. Riboflavin is beneficial for adults with methylenetetrahydrofolate (MTHFR) gene mutations.
- Niacin, Vitamin B3: niacin raises HDL, which helps remove the LDL from the arteries. HDL will remove extra cholesterol and plaque buildup in your arteries sending the arterial debris to the liver where the liver expels it from the body.
- Magnesium prevents muscle spasms in heart blood vessels. Further magnesium prevents calcium buildup in the cholesterol plaque in the arteries. Recall the stiffening of the arteries with plaque will occur as calcium is deposited in the arteries, rather than bones.
- Healthydirections.com is the website for Dr. Stephen Sinatra. Dr. Sinatra supports heart health with the use of Coenzyme Q10 (Ubiquinol), D-Ribose, and L-Arginine.
References
- American Journal of Clinical Nutrition, Vol. 72, Issue 5, Nov. 2000, PP 1307-1315
- Healthline, Oct. 27, 2021
- ACSM (2018). ACSM’s New Exercise Preparticipation Screening: Removing Barriers to Initiating Exercise. https://www.acsm.org/blog-detail/acsm-certified-blog/2018/02/01/exercise-preparticipation-screening-removing-barriers-initiating-exercise
- American College of Sports Medicine (2018). ACSM’s Guidelines for Exercise Testing and Prescription (10th ed.). Philadelphia: Wolters Kluwer.
- Riebe, D., Franklin, B.A., Thompson, P.D., Garber, C.E., Whitfield, G.P., Magal, M., & Pescatello, L.S. (2015). Updating ACSM’s Recommendations for Exercise Preparticipation Health Screening. Medicine & Science in Sports & Exercise, 48(3), 579.
- Whitfield, G., Gabriel, K., Rahbar, M., & Kohl, H. (2014). Application of the American Heart Association/American College of Sports Medicine Adult Preparticipation Screening Checklist to a Nationally Representative Sample of US Adults Aged ≥40 Years From the National Health and Nutrition Examination Survey 2001 to 2004. Circulation, 119, 1113-1120.