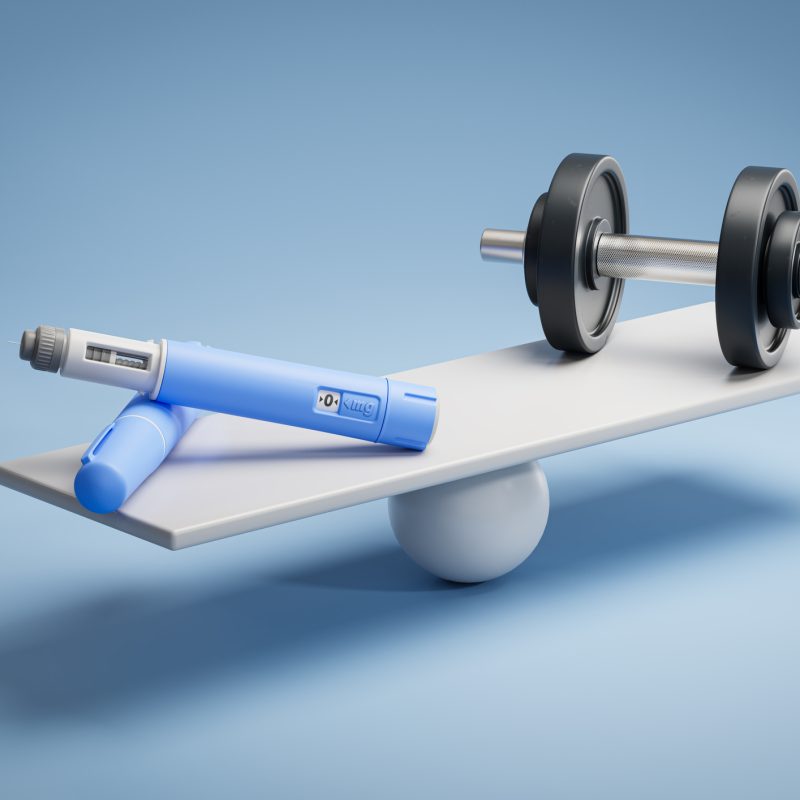
As the popularity of GLP-1 receptor agonists (GLP-1 RAs) continues to surge, particularly among clients seeking medically supported weight loss, personal trainers must evolve their programming frameworks to address a critical physiological challenge: the unintentional loss of skeletal muscle. While these medications effectively reduce body weight and improve glycemic control (Jiao et al., 2024), they also present a paradox: Specifically, clients may be shrinking the number on the scale but simultaneously losing metabolically active tissue essential for long-term health, function, and vitality.
This article offers evidence-informed strategies to mitigate that risk. By combining structured resistance training with intentional nutrition strategies, personal trainers can help preserve lean mass, support hormonal balance, and optimize body composition during GLP-1–induced weight loss. Whether working with beginners or seasoned exercisers, the solution is creating muscle-centric, client-specific training programs emphasizing volume, intensity, recovery, and sustainability.
Understanding the Mechanism: Muscle Loss and GLP-1 Use
Muscle loss during weight loss is not new, but the degree to which it occurs during GLP-1–mediated weight reduction has prompted fresh scrutiny. Studies show that while GLP-1 RAs such as liraglutide and semaglutide result in significant fat mass loss, they can also cause a concurrent decline in lean body mass (Old et al., 2025; Sargeant et al., 2019). This is particularly concerning in older adults or those with preexisting sarcopenia risk, where even modest muscle loss can impair mobility, increase fall risk, and reduce metabolic health (Beavers et al., 2013; Beaudart et al., 2014).
Consequently, exercise professionals are now tasked with designing programs that counteract these catabolic effects. Resistance training (RT)—long known for its role in muscle hypertrophy and strength—is emerging as a frontline strategy to maintain functional tissue integrity during medically induced weight loss (Bellicha et al., 2018).
Programming Foundations: Beginners vs. Intermediate Lifters
When working with GLP-1 users, it is essential to tailor resistance training protocols based on training status.
For Beginners:
Beginners often encounter multiple barriers: low confidence in exercise, medication-related fatigue, and reduced appetite. For these individuals, simplicity and consistency are essential. Full-body resistance training sessions, done two to three times a week, provide an ideal starting point. The main goal should be neuromuscular adaptation, focusing on teaching proper movement mechanics and building a foundation for progressive overload. Exercises should be compound in nature (like squats, hip hinges, pushes, and pulls) and performed at an intensity of 60–70% of 1RM for 2–3 sets of 10–12 reps.
For Intermediate Lifters:
Clients with prior lifting experience or baseline strength levels can safely benefit from higher intensities. Programs should incorporate progressive overload and periodization, alternating hypertrophy and strength-focused blocks. Training at or above 70% of 1RM has been shown to be particularly effective in preserving lean mass during caloric deficits (Shea et al., 2011; Roth et al., 2022). Intermediate lifters may benefit from 3–4 weekly sessions, with split routines that allow greater volume without compromising recovery.
The principle of minimal effective dose is especially important for GLP-1 users, as fatigue and gastrointestinal distress may be more pronounced. The goal is not maximum volume, but optimal stimulus. Specifically, just enough to activate muscle protein synthesis and preserve mass while respecting the client’s recovery capacity.
Volume, Intensity, and Recovery Considerations
Emerging research suggests that while high training volume can support hypertrophy in energy-balanced states, it may not confer additional lean mass preservation benefits under calorie restriction (Roth et al., 2022). Instead, training intensity (e.g., the percentage of 1RM used during work sets) appears to be a more influential factor in muscle retention during weight loss (Avila et al., 2010).
In general:
- Intensity: Aim for 65–85% of 1RM, depending on client experience.
- Volume: 2–4 sets per movement, focusing on multi-joint compound exercises.
- Frequency: 2–4x/week, allowing for 48–72 hours of recovery per muscle group.
- Tempo: Controlled eccentrics (2–3 seconds) to maximize time under tension.
Additionally, trainers should monitor signs of recovery issues, such as prolonged DOMS, poor sleep, decreased performance, or increased irritability, and modify the program as needed. Put another way, recovery is an active component of training programming, not a mere afterthought.
Special Considerations for GLP-1 Users: Fatigue, Hydration, and GI Tolerance
Clients on GLP-1 agonists often report nausea, dehydration, or fatigue, especially in the first 8–12 weeks of treatment (Osaka et al., 2023). These side effects can interfere with adherence and intensity, so trainers must adjust programs dynamically.
Key strategies include:
- Shorter Sessions: 30–45 minutes is often better tolerated than hour-long workouts.
- Warm-Up Emphasis: Low-intensity aerobic warm-ups and mobility work can help reduce nausea.
- Hydration Monitoring: Encourage consistent water intake before, during, and after sessions, especially on injection days.
- Low-GI Movement Days: Schedule lower-intensity resistance circuits or mobility work on days when GI symptoms are more pronounced.
Empathy and flexibility are key. A missed session isn’t a failure; instead, it’s a powerful form of instant feedback. As a result, Coaches should constantly monitor biofeedback and adapt training accordingly to promote long-term consistency.
Nutrient Timing and Protein Intake: The Appetite Suppression Puzzle
GLP-1 users often experience profound appetite suppression, which may hinder their ability to consume enough protein to support muscle maintenance. This presents a unique challenge for trainers, as inadequate protein intake undermines the anabolic stimulus of resistance training (Beavers et al., 2018).
Recommendations include:
- Target ≥1.2–1.6g protein/kg/day for muscle preservation (Mason et al., 2013).
- Distribute protein evenly across meals—aim for 20–40g per meal to maximize muscle protein synthesis.
- Use shakes or liquid supplements as needed, especially post-workout when solid food is unappealing.
- Educate clients on easy-to-digest, high-protein options (e.g., Greek yogurt, eggs, whey protein).
Trainers are not dietitians, but they can help clients troubleshoot logistics and identify barriers to adequate protein intake, working in partnership with healthcare professionals as needed.
Final Thoughts: Why Trainers Are More Important Than Ever
Ultimately, GLP-1 therapies are here to stay. While these therapies provide significant benefits for managing metabolic diseases, they also introduce new challenges: most notably, the unintended loss of muscle mass, which is crucial for maintaining health, vitality, and independence.
In this regard, personal trainers are uniquely positioned to contribute to the solution. By employing evidence-informed programming and compassionate coaching, we can assist clients in preserving functional strength, preventing sarcopenia, and optimizing health outcomes during medically supervised weight loss.
In summary, this goes beyond a mere clinical opportunity; it is a professional imperative. As the muscle-centric movement gains momentum, resistance training continues to evolve from being just a gym routine to a vital component of medical care. In this context, we, as trainers, become an essential part of the healthcare team.
References
Avila, J., Gutierres, J., Sheehy, M., Lofgren, I., & Delmonico, M. (2010). Effect of moderate intensity resistance training during weight loss on body composition and physical performance in overweight older adults. European Journal of Applied Physiology, 109(3), 517–525. https://doi.org/10.1007/s00421-010-1387-9
Beavers, K., Beavers, D., Nesbit, B., Ambrosius, W., Marsh, A., Nicklas, B., … & Rejeski, W. (2013). Effect of an 18-month physical activity and weight loss intervention on body composition in overweight and obese older adults. Obesity, 22(2), 325–331. https://doi.org/10.1002/oby.20607
Beavers, K., Nesbit, B., Kiel, J., Sheedy, J., Arterburn, L., Collins, A., … & Beavers, D. (2018). Effect of an energy-restricted, nutritionally complete, higher protein meal plan on body composition and mobility in older adults with obesity: A randomized controlled trial. The Journals of Gerontology Series A, 74(6), 929–935. https://doi.org/10.1093/gerona/gly146
Bellicha, A., Ciangura, C., Poitou, C., Portero, P., & Oppert, J. (2018). Effectiveness of exercise training after bariatric surgery—a systematic literature review and meta-analysis. Obesity Reviews, 19(11), 1544–1556. https://doi.org/10.1111/obr.12740
Jiao, R., Lin, C., Cai, X., Wang, J., Wang, Y., Lv, F., … & Ji, L. (2024). Characterizing body composition modifying effects of a glucagon-like peptide 1 receptor–based agonist: A meta-analysis. Diabetes, Obesity and Metabolism, 27(1), 259–267. https://doi.org/10.1111/dom.16012
Mason, C., Xiao, L., Imayama, I., Duggan, C., Foster-Schubert, K., Kong, A., … & McTiernan, A. (2013). Influence of diet, exercise, and serum vitamin D on sarcopenia in postmenopausal women. Medicine & Science in Sports & Exercise, 45(4), 607–614. https://doi.org/10.1249/mss.0b013e31827aa3fa
Old, V., Davies, M., Papamargaritis, D., Choudhary, P., & Watson, E. (2025). The effects of glucagon-like peptide-1 receptor agonists on mitochondrial function within skeletal muscle: A systematic review. Journal of Cachexia, Sarcopenia and Muscle, 16(1). https://doi.org/10.1002/jcsm.13677
Osaka, T., Hamaguchi, M., & Fukui, M. (2023). Favorable appendicular skeletal muscle mass changes in older patients with type 2 diabetes receiving GLP-1 receptor agonist and basal insulin co-therapy. Clinical Medicine Insights: Endocrinology and Diabetes, 16. https://doi.org/10.1177/11795514231161885
Roth, C., Schwiete, C., Happ, K., Rettenmaier, L., Schöenfeld, B., & Behringer, M. (2022). Resistance training volume does not influence lean mass preservation during energy restriction in trained males. Scandinavian Journal of Medicine and Science in Sports, 33(1), 20–35. https://doi.org/10.1111/sms.14237
Sargeant, J., Henson, J., King, J., Yates, T., Khunti, K., & Davies, M. (2019). A review of the effects of glucagon-like peptide-1 receptor agonists and sodium-glucose cotransporter 2 inhibitors on lean body mass in humans. Endocrinology and Metabolism, 34(3), 247. https://doi.org/10.3803/enm.2019.34.3.247
Shea, M., Nicklas, B., Marsh, A., Houston, D., Miller, G., Isom, S., … & Kritchevsky, S. (2011). The effect of pioglitazone and resistance training on body composition in older men and women undergoing hypocaloric weight loss. Obesity, 19(8), 1636–1646. https://doi.org/10.1038/oby.2010.327






