Gait can be a four-letter word with unfortunate consequences if one’s stride becomes disorderly or abnormal. Personal trainers who can perform a functional gait assessment will have the advantage of noting the following risk factors:
1. Gait assessment is likely to identify subjects at increased risk of falling.
2. Gait is a marker for otherwise undetected and perhaps treatable disease
3. Neurological gait disorders …are associated with recurrent falls, lower cognitive function, depressed mood, and diminished quality of life.
Who has the easy gait of an athlete?
One’s manner of walking can be effortless, or it can be laborious or even painful.
Hundreds of muscles and muscle groups, plus major joints and connective tissues and our central nervous system are involved in human locomotion. A professional trainer’s goal is to enhance that athletic locomotion when possible, to improve mobility, ease discomfort, help to prevent falls, and perhaps identify a neurological malady like Ataxia or Parkinson’s Disease (PD).
This column addresses:
1. how to gauge a client’s gait,
2. healthy biomechanics of walking,
3. notable gait disorders,
4. stretching, and
5. special considerations, including those for older clients (with their higher incidence of degenerative conditions in mind and body).
Gait – Strike One
By definition, gait is an individual’s manner of moving on two legs. (In contrast to jogging or running, walking/striding means that one foot is in contact with the ground surface through a full sequence.)
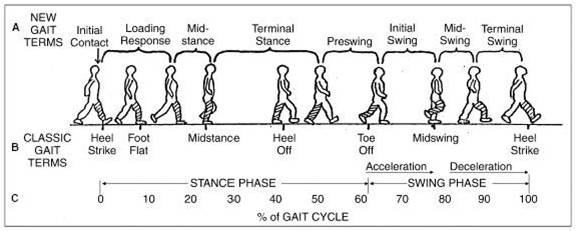
The illustrative series above shows an initial right heel strike for the stance phase of a walking stride with the left body side leading. The figure’s arms suggest a natural [opposite body side] swing as the swing phase of a stride is completed.
Striding for fitness and health is not Olympian speed-walking, forefoot (toe-strike) sprint actions. Shin splints or other discomforts may result from the initial toe or forefoot strikes, particularly if the older client is heavy in build.
Healthy Biomechanics
A trainer should be aware of these “best practices” for usual striding – for effective velocity and efficient injury prevention.
- Maintain a tall or long spine posture with a “proud” chest – without a forward head tilt.
- Keep eyes forward – not scanning upward or downward for too long.
- Breathe deep with diaphragm and optimal lung expansion.
- Relax the shoulder girdle.
- Keep a natural arm swing: not the exaggerated hip and arm swing of Olympic speed walking!
- Use regular stretching and stability exercises to maintain the Lumbo-Pelvic Hip Complex (LPHC) capacity for effective striding.
*Note: If a client’s lower or mid-back tightens when walkings, she/he should make subtle adjustments and pull “belly button against backbone” to properly activate key muscle deep core groups.
Learn more in our Functional Training Specialist as a part of our Continuing Education Course Series.
Notable Gait Disorders
Medical and biomechanics details of abnormal or disorderly gaits are beyond the scope of this post. Yet, a trainer should be fully aware (for clients of any age) when physical cues or verbal interactions suggest an issue.
Should an older client exhibit or mention slight imbalance or frustration with gait changes, or perhaps mention recent trips or falls, a formal Functional Gait Assessment (FGA) may be warranted.
A trainer may use this practical gait assessment to gauge a client’s fitness performance in ten (10) vital walking measures and contexts:
- Gait on a level surface (good speed, no bodily imbalance, and/or minimal deviation from a straight walking path).
- Change in gait speed (The goal is no significant gait impairments or deviations between a client’s normal, fast, and slow speeds.) Of note, gait speed is a reliable indicator of longevity.
- Maintain a gait with horizontal head turns (Proprioception or a client’s spatial awareness for factors 3-10 below.)
- Maintain a gait with vertical head turns.
- The quickness of gait with a safe pivot turn of 180 degrees.
- Dealing with obstacles in the client’s path.
- Gait with a narrow base of support (Arms crossed, heel to toe strides as if taking a sobriety test.)
- Forward gait stability with eyes closed.
- Backward gait with eyes open.
- Walking up and down stairs or steps (without hands-on rails).
Both trainers and clients should appreciate the validated need to get about safely under these ten varied conditions. Helping a client maintain acute proprioception is an implicit goal for trainers that work with aging clients (> 70 years of age).
Think fall prevention. Think quality of life.
Pre and Post Stretches
A client’s pre-and post-walking stretches are often a matter of preference.
Yet, increasing ranges of motion for efficient strides and preventing injury are assured reasons for stretching.
It is a good practice for a client to make the first segment (~10 minutes) the slowest for the walk, serving as a dynamic stretch to prevent injury and improve performance.
Post-walk static stretches of 20 to 30 seconds per stretch for the lower limb, core and upper body segments are very useful, such as a World’s Greatest Stretch (below):.
Special Considerations
Common client questions may crop up when walking for stamina, stretching and stability are discussed. Three possible topics are:
May I use a backpack or fanny pack?
Comfortable and well-fitting packs are encouraged for nature hikes, as first aid items, water, and snacks are appropriate for longer excursions.
How about wrist weights?
One to 5-pound “Velcro’ed” (hook and loop) weights can be used to increase loading for a client’s arms, shoulders, and back.
- Adding moderate (not heavy) resistance efforts improve caloric burn and help maintain muscle tone.
Yet, the key is to accommodate the added weights without perturbing the client’s normal gait or stride.
Canes or walking sticks?
Trainers should situationally assess whether a client’s use of a cane or walking/hiking stick is a help or hindrance to a “normal” gait. It is certainly better for a client who needs a cane to walk to use it, rather than remain sedentary.
Older Client Considerations
As clients age (with age 70 as a nominal tipping point), it is a valid general statement that neuromuscular interactions diminish. With inevitable effect of advanced age, safe and fun activities of daily life that involve mobility can be compromised.
Examples:
- A woman with osteoporosis will likely have more severe gait issues that others.
- If a client experiences multiple disorders, perhaps a combination of ataxia and advanced sarcopenia, her or his chances of falling are heightened.
An adage which Queen Elizabeth used at her spry age of 95 is fitting, “when you stop, you drop…” Accommodations can and should be used to promote ambulatory motion for as long as possible (possibly under medical guidance/supervision).
Getting from point A to point B is a simple yet hard motivation for some to use “motion as medicine.”
A fair percentage of elders – possibly one-quarter of them – have nature/nurture on their sides to avoid significant gait issues.
Summary
Human gait is not by any measure a simple process. Yet, it is an under-appreciated enabler for activities of daily life for all our clients. Thus, we trainers should be fully aware of potential disorders from normal Gaits which may be neurological, biomechanics, or sadly both.
Bear in mind that:
- A client’s gait is influenced by age, personality, mood, and social factors.
- Preferred walking speed in older adults is a viable marker of longevity.
- Gait disorders can lead to a loss of personal freedom, increase falls, and possible injuries.
Functional Gait Assessments (FGAs) are credible ways in which to gauge a client’s proprioception, and to mark possible CNS and biomechanics abnormalities.
References
- https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0069627






